Coronary Angioplasty
Home - Coronary Angioplasty
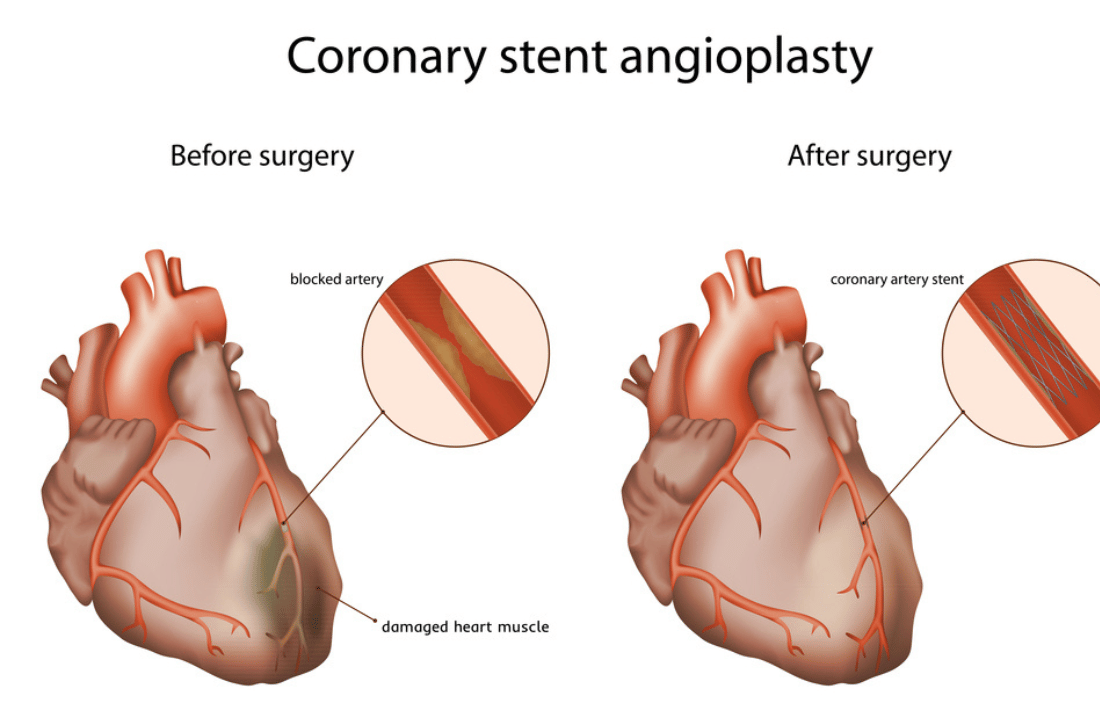
Coronary Angioplasty, also known as Percutaneous Coronary Intervention (PCI), is a minimally invasive procedure used to treat coronary artery disease (CAD) by opening blocked or narrowed coronary arteries. This procedure plays a crucial role in improving blood flow to the heart muscle, alleviating symptoms such as chest pain (angina), and reducing the risk of heart attack.
Understanding Coronary Artery Disease (CAD)
Coronary artery disease (CAD) occurs when the coronary arteries, which supply oxygen-rich blood to the heart, become narrowed or blocked due to the buildup of cholesterol plaque. This narrowing can restrict blood flow to the heart muscle, leading to symptoms such as angina, shortness of breath, and in severe cases, heart attack.
Risk Factors for CAD
Several factors increase the risk of developing coronary artery disease:
- High Cholesterol: Elevated levels of LDL (“bad”) cholesterol and low levels of HDL (“good”) cholesterol contribute to plaque buildup in the arteries.
- Hypertension: High blood pressure puts stress on the artery walls, accelerating the formation of plaque.
- Smoking: Tobacco use damages the lining of the arteries and increases the risk of plaque buildup.
- Diabetes: Diabetes mellitus increases the risk of cardiovascular disease by affecting blood sugar levels and metabolism.
- Family History: Individuals with a family history of heart disease are at higher risk due to genetic factors.
- Obesity and Sedentary Lifestyle: Lack of physical activity and excess body weight contribute to the development of CAD.
Indications for Coronary Angioplasty
Coronary Angioplasty is recommended for patients with:
- Symptomatic Coronary Artery Disease: Patients experiencing angina (chest pain) or other symptoms of reduced blood flow to the heart.
- Acute Coronary Syndrome: Including unstable angina or myocardial infarction (heart attack), where prompt restoration of blood flow is critical.
- Significant Coronary Artery Blockages: Identified during Coronary Angiography, indicating the need for intervention to prevent complications and improve heart function.
Types of Coronary Angioplasty Procedures
Balloon Angioplasty
Balloon Angioplasty involves inflating a balloon at the tip of a catheter to compress plaque against the artery walls and widen the narrowed segment. This procedure alone may be sufficient for minor blockages or as a preliminary step before stent placement.
Stent Placement
Stents are small, expandable mesh tubes inserted into the coronary artery to help keep it open and maintain blood flow. There are two main types of stents:
- Bare Metal Stents (BMS): Provide structural support to the artery but may be associated with a higher risk of re-narrowing (restenosis).
- Drug-Eluting Stents (DES): Coated with medication that slowly releases to prevent scar tissue formation and reduce the risk of restenosis.
Drug-Coated Balloon Angioplasty
A newer approach involves using a balloon coated with medication to deliver drugs directly to the artery wall during inflation. This technique can help prevent restenosis and may be used in combination with or instead of stent placement.
Advancements in Coronary Angioplasty Techniques
Fractional Flow Reserve (FFR)
FFR is a measurement used during Coronary Angiography to assess the severity of coronary artery blockages. It involves inserting a pressure wire into the coronary artery to measure blood pressure and determine whether a blockage requires treatment.
Intravascular Ultrasound (IVUS)
IVUS uses sound waves to create detailed images of the inside of coronary arteries, providing cardiologists with enhanced visualization to guide precise placement of stents and assess vessel wall characteristics.
Optical Coherence Tomography (OCT)
OCT utilizes light waves to generate high-resolution images of coronary arteries, allowing for detailed assessment of plaque characteristics and optimal stent deployment.
Benefits of Coronary Angioplasty
Coronary Angioplasty offers several benefits for patients with coronary artery disease:
- Improved Symptoms: Many patients experience immediate relief from angina and increased exercise tolerance.
- Reduced Risk of Heart Attack: By restoring blood flow to the heart muscle, Coronary Angioplasty lowers the risk of myocardial infarction and other cardiac events.
- Enhanced Quality of Life: Patients report improved quality of life, reduced hospitalizations, and increased ability to perform daily activities.
Risks and Complications
While Coronary Angioplasty is generally safe, it carries some risks, including:
- Bleeding or Hematoma: At the catheter insertion site in the groin or wrist.
- Allergic Reactions: To medications or contrast dye used during the procedure.
- Coronary Artery Dissection: A tear in the artery wall, requiring additional intervention.
- Restenosis: Recurrence of narrowing within the treated artery, particularly with bare metal stents.
- Rare Complications: Such as heart rhythm disturbances or kidney damage due to contrast dye.
Preparation for Coronary Angioplasty
Pre-Procedure Evaluation
Before Coronary Angioplasty, your healthcare team will conduct a comprehensive evaluation, including:
- Medical History Review: Assessing your symptoms, cardiovascular risk factors, and prior cardiac interventions.
- Physical Examination: To evaluate your overall health and readiness for the procedure.
- Diagnostic Tests: Such as an Electrocardiogram (ECG), Echocardiogram, or Stress Test, to assess heart function and identify any underlying conditions.
Medication Management
You may be instructed to adjust medications before Coronary Angioplasty, particularly blood thinners or medications that affect blood sugar levels. It’s essential to follow your cardiologist’s instructions closely to optimize procedure outcomes.
Fasting Guidelines
You will typically be asked to fast for several hours before the procedure to reduce the risk of complications associated with anaesthesia and sedatives. Your healthcare provider will provide specific fasting instructions based on your individual needs.
Preparation for Coronary Angioplasty
Pre-Procedure Evaluation
Before Coronary Angioplasty, your healthcare team will conduct a comprehensive evaluation, including:
- Medical History Review: Assessing your symptoms, cardiovascular risk factors, and prior cardiac interventions.
- Physical Examination: To evaluate your overall health and readiness for the procedure.
- Diagnostic Tests: Such as an Electrocardiogram (ECG), Echocardiogram, or Stress Test, to assess heart function and identify any underlying conditions.
Medication Management
You may be instructed to adjust medications before Coronary Angioplasty, particularly blood thinners or medications that affect blood sugar levels. It’s essential to follow your cardiologist’s instructions closely to optimize procedure outcomes.
Fasting Guidelines
You will typically be asked to fast for several hours before the procedure to reduce the risk of complications associated with anaesthesia and sedatives. Your healthcare provider will provide specific fasting instructions based on your individual needs.
What to Expect During Coronary Angioplasty
Procedure Setting
Coronary Angioplasty is performed in a specialized cardiac catheterization laboratory (cath lab) equipped with advanced imaging technology and monitoring equipment. You will be positioned on an examination table, and local anaesthesia will be administered at the catheter insertion site to ensure your comfort throughout the procedure.
Catheter Insertion and Imaging
- Groin or Wrist Access: A small incision is made at the chosen insertion site (groin or wrist), and a catheter is carefully threaded through the blood vessel to reach the coronary arteries under fluoroscopic guidance.
- Contrast Injection: Once the catheter is in place, a contrast dye is injected into the coronary arteries to visualize any blockages or narrowing on X-ray images (angiograms).
- Balloon Inflation and Stent Deployment: If necessary, the balloon at the catheter’s tip is inflated to compress the plaque against the artery walls and widen the artery. A stent may then be deployed to support the artery and maintain adequate blood flow.
Monitoring and Recovery
During Coronary Angioplasty, you will be closely monitored by a team of interventional cardiologists, nurses, and technologists. Vital signs, such as blood pressure and heart rate, will be continuously monitored to ensure your safety and well-being throughout the procedure.
Post-Procedural Care and Recovery
Immediate Recovery
After Coronary Angioplasty, you will be transferred to a recovery area where your vital signs will continue to be monitored closely. You may experience mild discomfort at the catheter insertion site, which is typically managed with pain medications and compression bandages.
Hospital Stay
Most patients who undergo uncomplicated Coronary Angioplasty can expect to stay overnight for observation and monitoring. Your healthcare team will provide instructions on post-procedural care, including medication management, wound care (if applicable), and activity restrictions.
Follow-Up Appointments
You will be scheduled for follow-up appointments with your cardiologist to monitor your recovery and assess the effectiveness of Coronary Angioplasty. These appointments may include additional tests, such as repeat angiography or non-invasive imaging, to evaluate the treated coronary artery and overall heart function.
Advanced Technology and Expertise
Coronary angioplasty is performed by a multidisciplinary Dr Ankeet Dedhiya and his team of board-certified interventional cardiologists, nurses, and technologists. Our catheterization laboratory is equipped with state-of-the-art digital imaging technology, including intravascular ultrasound (IVUS) and optical coherence tomography (OCT), to ensure precise procedural guidance and optimal patient outcomes.
Patient Education and Support
Patient-Centered Care Approach
Before Coronary Angioplasty, you will receive comprehensive education about the procedure, including its benefits, risks, and expected outcomes. Our dedicated healthcare team is committed to supporting you throughout every step of your treatment journey, addressing any questions or concerns you may have.
Lifestyle Recommendations
Following Coronary Angioplasty, adopting a heart-healthy lifestyle can further improve your cardiovascular health and reduce the risk of future heart problems. Your cardiologist may recommend:
- Medication Adherence: Taking prescribed medications as directed to manage cholesterol levels, and blood pressure, and prevent blood clot formation.
- Healthy Diet: Incorporating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins to support heart health.
- Regular Physical Activity: Engaging in regular exercise, as recommended by your healthcare provider, to improve cardiovascular fitness and overall well-being.
- Smoking Cessation: Quitting smoking and avoiding secondhand smoke to reduce the risk of further damage to the coronary arteries.
Conclusion
Coronary Angioplasty is a transformative procedure that restores blood flow to the heart and improves the quality of life for patients with coronary artery disease. Dr Ankeet Dedhiya and his team are dedicated to providing compassionate, patient-centred care and utilizing advanced technology to achieve optimal outcomes. Whether you are seeking treatment for angina symptoms or recovering from a heart attack, our experienced team is here to support you on your journey to heart health.
FAQ
Frequently Asked Questions
Coronary Angioplasty, also known as Percutaneous Coronary Intervention (PCI), is a minimally invasive procedure used to open blocked or narrowed coronary arteries. It is often performed immediately following Coronary Angiography to restore blood flow to the heart muscle and alleviate symptoms of coronary artery disease (CAD).
Coronary Angioplasty is recommended for individuals who:
- Have significant blockages or narrowing in their coronary arteries identified during Coronary Angiography.
- Experience symptoms of angina (chest pain) or shortness of breath due to reduced blood flow to the heart.
- Have had a heart attack (myocardial infarction) to restore blood flow and prevent further damage to the heart muscle.
During Coronary Angioplasty:
- A catheter with a deflated balloon at its tip is inserted into a blood vessel in the groin or wrist and guided to the blocked coronary artery.
- Once in place, the balloon is inflated to compress the plaque buildup and widen the artery, restoring blood flow.
- In some cases, a stent (a small mesh tube) may be inserted and expanded to help keep the artery open.
Coronary Angioplasty is considered a safe procedure when performed by experienced cardiologists in a controlled clinical setting. Potential risks include bleeding at the catheter insertion site, allergic reactions to medications or contrast dye, and rare complications such as coronary artery dissection or heart rhythm disturbances.
Preparation typically includes:
- Fasting for several hours before the procedure, as advised by your healthcare provider.
- Informing your doctor about any medications you are taking, including blood thinners, as they may need to be adjusted before the procedure.
- Arranging for transportation home after the procedure, as you may be advised to rest for a short period following Coronary Angioplasty.
- During the Procedure: You will receive local anesthesia at the catheter insertion site to minimize discomfort. The procedure itself may take up to an hour, during which you will be closely monitored.
- After the Procedure: You will be monitored in a recovery area to ensure stability before discharge. Most patients can resume normal activities within a day, although strenuous activities may need to be avoided initially.
Following Coronary Angioplasty, your cardiologist will discuss:
- Improved blood flow to the heart and relief of symptoms such as chest pain (angina).
- Reduced risk of heart attack and other complications associated with coronary artery disease.
- Long-term management strategies, including medication, lifestyle changes, and follow-up appointments to monitor your heart health.
Many patients experience immediate relief from symptoms such as chest pain (angina) following Coronary Angioplasty. The procedure is designed to restore blood flow to the heart muscle quickly, improving overall cardiac function and reducing the risk of future cardiovascular events.
Depending on your medical history and specific circumstances, alternatives may include medications to manage symptoms, lifestyle changes to reduce risk factors, or coronary artery bypass grafting (CABG) for more extensive coronary artery disease. Your cardiologist will recommend the most appropriate treatment approach based on your individual needs.
To schedule a Coronary Angioplasty or learn more about the procedure, including insurance coverage and preparation guidelines, please contact [Dr Ankeet Dedhiya]. Our dedicated cardiovascular team is committed to providing compassionate care and personalized treatment options to optimize your heart health.