Peripheral Interventions
Home - Peripheral Interventions
Peripheral interventions encompass a range of minimally invasive procedures aimed at diagnosing and treating conditions affecting the peripheral arteries and veins. These procedures are vital in managing peripheral artery disease (PAD), deep vein thrombosis (DVT), and other vascular conditions, enhancing blood flow, alleviating symptoms, and improving patients’ quality of life.
Understanding Peripheral Artery Disease (PAD)
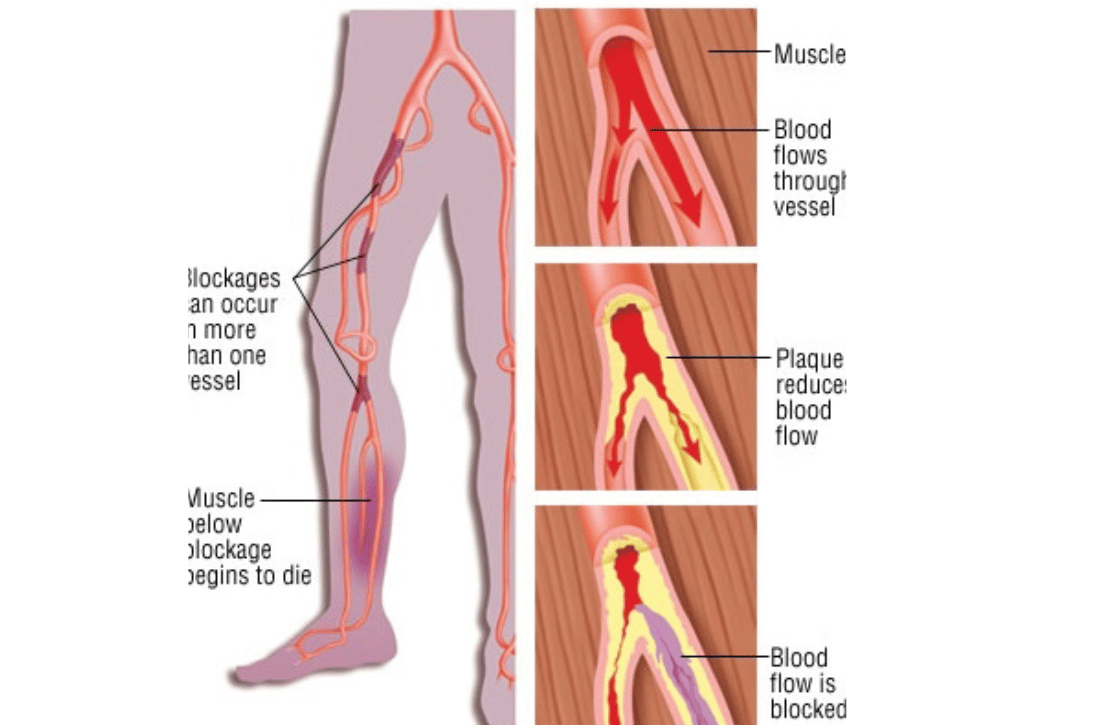
Peripheral artery disease is a common circulatory problem in which narrowed arteries reduce blood flow to the limbs. This condition, primarily affecting the legs, can lead to pain, mobility issues, and in severe cases, tissue damage and amputation.
Causes of PAD
- Atherosclerosis: The buildup of fatty deposits (plaque) in the artery walls, leading to narrowed or blocked arteries.
- Smoking: A significant risk factor that contributes to the development and progression of PAD.
- Diabetes: Elevated blood sugar levels damage blood vessels and contribute to atherosclerosis.
- Hypertension and Hyperlipidemia: High blood pressure and high cholesterol levels increase the risk of artery damage and plaque formation.
Symptoms of PAD
- Claudication: Pain or cramping in the legs triggered by walking or exercise, relieved by rest.
- Rest Pain: Persistent pain in the legs or feet, even at rest, indicating severe arterial blockage.
- Wounds and Ulcers: Slow-healing sores or ulcers on the legs and feet due to poor circulation.
- Cold and Discolored Limbs: Affected limbs may appear pale, blue, or feel cold to the touch.
Types of Peripheral Interventions
Peripheral interventions are designed to restore blood flow and alleviate symptoms associated with PAD and other vascular conditions. Key types of peripheral interventions include:
Angioplasty and Stenting
- Balloon Angioplasty: A catheter with a small balloon is inserted into the narrowed artery. The balloon is inflated to widen the artery and improve blood flow.
- Stent Placement: Following angioplasty, a stent (a small mesh tube) is placed in the artery to keep it open and prevent re-narrowing.
Atherectomy
- Directional Atherectomy: A catheter with a cutting blade or rotating burr is used to remove plaque from the artery walls, improving blood flow.
- Rotational Atherectomy: A high-speed rotating device grinds away calcified plaque, restoring vessel patency.
Thrombolysis and Thrombectomy
- Thrombolysis: Medications are delivered through a catheter to dissolve blood clots blocking the artery or vein.
- Thrombectomy: A catheter-based device is used to physically remove blood clots, restoring blood flow.
Endovascular Aneurysm Repair (EVAR)
- EVAR: A minimally invasive procedure to treat abdominal aortic aneurysms. A stent graft is placed within the aneurysm to reinforce the weakened artery wall and prevent rupture.
Benefits of Peripheral Interventions
- Minimally Invasive: Reduced risk of complications, shorter recovery times, and less post-procedural pain compared to open surgery.
- Symptom Relief: Significant improvement in symptoms such as pain, cramping, and mobility issues, enhancing quality of life.
- Improved Blood Flow: Restores adequate blood circulation to affected limbs, promoting healing of wounds and ulcers.
- Prevention of Severe Complications: Early intervention can prevent severe complications such as tissue loss, gangrene, and amputation.
Preparing for Peripheral Interventions
Pre-Procedure Evaluation
- Diagnostic Imaging: Ultrasound, CT angiography, or MR angiography to visualize the affected arteries and plan the intervention.
- Medical History and Physical Examination: Comprehensive assessment to determine the patient’s suitability for the procedure.
- Medication Review: Review of current medications, including blood thinners and anti-platelet agents, to minimize bleeding risks.
Procedure Steps
- Anaesthesia: Local anaesthesia or sedation is administered to ensure patient comfort during the procedure.
- Catheter Insertion: A small incision is made at the access site (typically in the groin or arm) to insert the catheter into the blood vessel.
- Guided Navigation: Using imaging techniques, the catheter is guided to the target site within the affected artery or vein.
- Intervention: The chosen intervention (e.g., angioplasty, stenting, atherectomy) is performed to restore blood flow.
- Closure: Once the procedure is completed, the catheter is removed, and the access site is closed with sutures or a closure device.
Post-Procedure Care
- Monitoring: Patients are closely monitored for any immediate complications such as bleeding, pain, or changes in limb circulation.
- Medications: Prescription of medications to prevent blood clots, reduce inflammation, and manage pain.
- Follow-Up: Scheduled follow-up appointments to assess the success of the intervention, monitor for restenosis, and address any ongoing symptoms.
Conclusion
Peripheral interventions are a cornerstone of modern vascular care, offering minimally invasive solutions for conditions such as peripheral artery disease, deep vein thrombosis, and aneurysms. Dr. Ankeet Dedhiya and our team of experienced interventional cardiologists and vascular specialists are dedicated to providing personalized, state-of-the-art care to improve your vascular health and quality of life. Whether you are undergoing diagnostic evaluation or preparing for a peripheral intervention, we are here to support you every step of the way.”
FAQ
Frequently Asked Questions
Peripheral interventions are minimally invasive procedures designed to diagnose and treat conditions affecting the peripheral arteries and veins. These procedures aim to improve blood flow, alleviate symptoms, and enhance the quality of life for patients with conditions such as peripheral artery disease (PAD) and deep vein thrombosis (DVT).
Peripheral interventions are recommended for patients with significant peripheral artery disease (PAD), deep vein thrombosis (DVT), or other vascular conditions that cause symptoms like pain, cramping, mobility issues, and poor wound healing. These procedures are also used to treat aneurysms and prevent severe complications such as tissue damage and amputation.
Peripheral artery disease is primarily caused by atherosclerosis, a condition where fatty deposits (plaque) build up in the artery walls, leading to narrowed or blocked arteries. Other risk factors include smoking, diabetes, hypertension, and high cholesterol levels.
Common symptoms of PAD include:
- Claudication: Pain or cramping in the legs triggered by walking or exercise, relieved by rest.
- Rest Pain: Persistent pain in the legs or feet, even at rest, indicating severe arterial blockage.
- Wounds and Ulcers: Slow-healing sores or ulcers on the legs and feet due to poor circulation.
- Cold and Discolored Limbs: Affected limbs may appear pale, blue, or feel cold to the touch.
Key types of peripheral interventions include:
- Angioplasty and Stenting: Procedures to widen narrowed arteries and keep them open using balloons and stents.
- Atherectomy: Techniques to remove plaque from artery walls using cutting blades or rotating devices.
- Thrombolysis and Thrombectomy: Methods to dissolve or physically remove blood clots blocking arteries or veins.
- Endovascular Aneurysm Repair (EVAR): A procedure to treat abdominal aortic aneurysms by placing a stent graft within the aneurysm.
Benefits include:
- Minimally Invasive: Reduced risk of complications, shorter recovery times, and less post-procedural pain compared to open surgery.
- Symptom Relief: Significant improvement in symptoms such as pain, cramping, and mobility issues, enhancing quality of life.
- Improved Blood Flow: Restores adequate blood circulation to affected limbs, promoting healing of wounds and ulcers.
- Prevention of Severe Complications: Early intervention can prevent severe complications such as tissue loss, gangrene, and amputation
While generally safe, peripheral interventions carry some risks, including:
- Bleeding and Hematoma: Blood vessel injury at the catheter insertion site may cause bleeding or hematoma formation.
- Arterial Dissection: Accidental tearing of the artery wall during the procedure, potentially requiring additional intervention.
- Restenosis: Re-narrowing of the treated artery over time, necessitating repeat intervention.
Infection: Risk of infection at the catheter insertion site or within the treated vessel.
- Diagnostic Imaging: Ultrasound, CT angiography, or MR angiography to visualize the affected arteries and plan the intervention.
- Medical History and Physical Examination: Comprehensive assessment to determine the patient's suitability for the procedure.
- Medication Review: Review of current medications, including blood thinners and antiplatelet agents, to minimize bleeding risks.
Procedure steps typically include:
- Anesthesia: Local anesthesia or sedation to ensure patient comfort.
- Catheter Insertion: A small incision is made to insert the catheter into the blood vessel.
- Guided Navigation: Using imaging techniques, the catheter is guided to the target site.
- Intervention: The chosen intervention (e.g., angioplasty, stenting, atherectomy) is performed to restore blood flow.
- Closure: The catheter is removed, and the access site is closed with sutures or a closure device.
Recovery involves:
- Monitoring: Close observation for any immediate complications such as bleeding or changes in limb circulation.
- Medications: Prescription of medications to prevent blood clots, reduce inflammation, and manage pain.
- Follow-Up: Scheduled follow-up appointments to assess the success of the intervention, monitor for restenosis, and address any ongoing symptoms.
Peripheral interventions are highly effective in improving blood flow, relieving symptoms, and preventing severe complications associated with PAD and other vascular conditions. The success of the procedure depends on the extent of the disease and the patient's overall health.
Yes, adopting a heart-healthy lifestyle can help maintain the success of the intervention and prevent further vascular issues:
- Quit Smoking: Smoking cessation is crucial for vascular health.
- Manage Chronic Conditions: Control diabetes, hypertension, and high cholesterol levels.
- Healthy Diet and Exercise: Maintain a balanced diet and engage in regular physical activity.
- Regular Monitoring: Keep up with follow-up appointments and monitor any changes in symptoms.